What are Hemorrhoids?
Hemorrhoids, also known as piles, are swollen or enlarged blood vessels inside or around the rectum and anus. When veins in the lining of the anus and rectum become enlarged, they are filled with excess blood and cause the underlying tissues to swell, forming abnormal lumps. Hemorrhoids may be caused due to excessive abdominal pressure from standing or sitting for long periods, obesity, pregnancy, and straining during constipation. Signs and symptoms include persistent pain, swelling, itching, burning and bleeding in the anal area.
There are various non-surgical and surgical methods employed to treat hemorrhoids.
Grades and Classifications of Hemorrhoids
Hemorrhoids are graded and classified on the basis of their location and the degree of prolapse (abnormal protrusion).
- Grade 1 hemorrhoids are small inflammations inside the anus and are not visible.
- Grade 2 hemorrhoids are also located inside the anus but prolapse outside the anal canal when passing stool and retract voluntarily.
- Grade 3 hemorrhoids appear prolapsed outside the anus but can be manually reduced.
- Grade 4 hemorrhoids are irreducible and appear always prolapsed.
Hemorrhoids are classified into two types:
- Internal Hemorrhoids: These are swellings that develop inside the anus. You may not be able to see or feel them. Sometimes, they may protrude through the anus to form external hemorrhoids.
- External Hemorrhoids: These are swellings that develop outside the anus while passing stools. You may be able to see and feel them. External hemorrhoids involving blood clots are called thrombosed hemorrhoids and are extremely painful.
Indications for Hemorrhoid Treatments
Hemorrhoids usually do not require treatment as the signs and symptoms often resolve on their own after a few days. However, based on the severity of the hemorrhoids and the persistence of signs and symptoms, several types of treatment measures are indicated accordingly.
Hemorrhoid Treatments
The different types of treatment measures employed for the management of hemorrhoids include:
Dietary and lifestyle modifications
If the main cause for the formation of hemorrhoids is constipation, the first line of treatment usually involves softening and regularising stools. The symptoms of hemorrhoids can often be relieved with dietary changes and lifestyle modifications. A high-fiber diet, including fruits, vegetables, whole-grain cereals, and bread can help to soften stools and avoid straining. Your doctor will also advise you to increase your water consumption and exercise regularly to avoid constipation. Soaking in warm bathtub water for 10 minutes several times a day may also provide relief.
Medications
Your doctor may suggest short-term remedies such as over-the-counter creams, ointments, or suppositories to relieve pain, swelling, inflammation, and itching. Avoid relying on them for a prolonged period, as they may damage the skin around your anus. Your doctor may prescribe pain killers to treat painful hemorrhoids, and laxatives to soften stools and empty your bowels.
Minimally invasive procedures
When a blood clot forms in external hemorrhoids, your doctor will make a small incision and remove the clot. Hemorrhoids that are painful, and bleed continuously may be treated with minimally invasive procedures. These include:
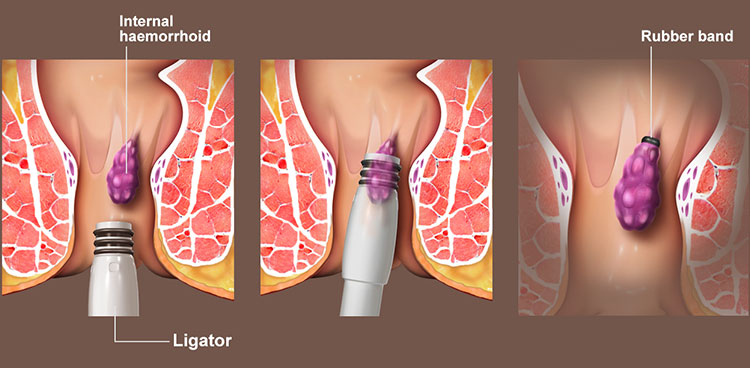
- Rubber band ligation: A rubber band is tied around the base of hemorrhoid to cut off the blood supply, so they disappear in a few days. This may be performed in your doctor’s office without the need for anesthesia.
- Injection (sclerotherapy): Your doctor will inject a chemical solution into the hemorrhoids. This relieves pain and hardens the Hemorrhoidal tissue to form a scar. This shrinks hemorrhoids in 4 to 6 weeks.
- Coagulation technique: Laser, infrared light or heat may be used to burn off the Hemorrhoidal tissue. These coagulation techniques cut off the blood supply, causing the small internal hemorrhoids to harden and shrink.
Surgical procedures
Your doctor may suggest surgery if the hemorrhoids are large and are not successfully treated with other procedures.
- Hemorrhoid removal (Hemorrhoidectomy): Your doctor will open the anus and surgically remove the hemorrhoids. This is the most effective treatment option for recurring or severe hemorrhoids.
- Stapled Hemorrhoidopexy: This procedure is mainly performed to treat hemorrhoids that hang out of the anus. The hemorrhoids will be stapled to the wall of the anal canal, which will reduce blood circulation and shrink them.
- Hemorrhoidal artery ligation: Your doctor will identify the artery supplying blood to the hemorrhoids with the help of an ultrasound probe. Blood supply to the identified artery will be blocked, which will help shrink the hemorrhoids.
Preparation for Hemorrhoid Treatments
Preoperative preparation for hemorrhoid treatment will involve the following steps:
- A thorough examination by your doctor to check for any medical issues that need to be addressed prior to surgery.
- Depending on your medical history, social history, and age, you may need to undergo tests such as blood work and imaging to help detect any abnormalities that could threaten the safety of the procedure.
- You should avoid supplements or medications such as blood thinners, aspirin, NSAIDs (non-steroidal anti-inflammatory drugs), or vitamin E for 1 to 2 weeks prior to surgery.
- You will be asked if you have allergies to medications, anesthesia, or latex.
- You should inform your doctor of any medications, vitamins, or supplements you are taking.
- You should refrain from alcohol or tobacco for at least 24 hours prior to surgery.
- You should not consume any solids or liquids for at least 8 hours prior to surgery.
- You may be given a laxative or enema to clear your bowel prior to surgery.
- Arrange for someone to drive you home as you will be groggy post-surgery.
- A written consent will be obtained from you after the surgical procedure has been explained in detail.
Postoperative Care Instructions and Recovery
In general, postoperative care instructions and recovery after hemorrhoid surgery will involve the following steps:
- You will be transferred to the recovery area to be monitored until you are awake from the anesthesia.
- Your nurse will monitor your wound and vital signs for the first few hours as you recover.
- You will normally be able to get out of bed and walk after a few hours with assistance.
- Retain the dressing over the site of surgery for a day or two; the dressing is most likely to come off by itself.
- The wound will be moist for a week or two and you may feel soreness for a few days. You can also expect some yellow discharge and bleeding for at least a week.
- Pain medications or NSAIDs will be prescribed to manage pain, drainage, or any discomfort.
- Antibiotics may be prescribed for any risk of infection associated with surgery.
- You will probably be given stool softeners or laxatives to prevent constipation and reduce discomfort in emptying your bowels.
- Instructions on surgical site care, bathing, driving, and resumption of sexual activity will be provided.
- You need to take off from work for at least a week or two to recover. You will be able to return to work and resume all your normal activities in 1 to 2 weeks.
- Refrain from strenuous activities or heavy lifting for at least a week.
- Maintain a healthy high fiber diet that includes lots of fruits and vegetables and drink plenty of water to assist with the smooth passing of stools.
- Avoid foods that promote constipation such as processed foods, sugary foods, caffeinated drinks, dairy products, and red meat.
- Refrain from smoking as it can negatively affect the healing process.
- A follow-up appointment will be scheduled to monitor your progress.
Risks and Complications of Hemorrhoid Treatments
Any procedures associated with hemorrhoid treatments are relatively safe; however, as with any procedure, there are risks and complications that could occur, such as:
- Persistent pain
- Bleeding and drainage
- Infection
- Injury to sphincter muscles
- Inflammation
- Difficulty urinating
- Stenosis (narrowing of the anus opening)





